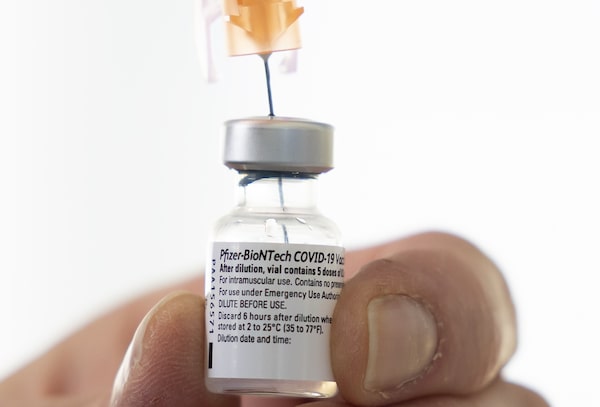
A dose of the Pfizer-BioNTech COVID-19 vaccine at a vaccination site in Vancouver on March 11, 2021.JONATHAN HAYWARD/The Canadian Press
Efficacy, blood clots, fetal cells, age restrictions, one shot or two, allergies and more.
The barrage of headlines about coronavirus vaccines can be overwhelming. It’s almost enough to make you think that getting a vaccine is more risky than not getting one.
So let’s start with the big picture.
Just one year after COVID-19 was declared a pandemic, almost a dozen vaccines have been tested and approved around the world – an unparalleled feat of science. To date, 360 million people worldwide have been vaccinated, and that’s increasing by about 10 million daily. Despite a slow start, more than three million Canadians have now been vaccinated.
One of the big questions people are now considering is whether one vaccine is better than the others.
Canada pre-purchased millions of doses of seven different vaccine types, and Health Canada has approved four so far for the various provincial and territorial rollouts. All the drugs are fully effective in preventing serious illness and death, though some may do more than others to stop any symptomatic illness at all (which is where the efficacy rates cited below come in).
- Also known as: Comirnaty
- Approved on: Dec. 9, 2020
- Efficacy rate: 95 per cent with both doses in patients 16 and older, and 100 per cent in 12- to 15-year-olds
- Traits: Must be stored at -70 C, requiring specialized ultracold freezers. It is a new type of mRNA-based vaccine that gives the body a sample of the virus’s DNA to teach immune systems how to fight it. Health Canada has authorized it for use in people as young as 12.
- Also known as: SpikeVax
- Approved on: Dec. 23, 2020
- Efficacy rate: 94 per cent with both doses in patients 18 and older, and 100 per cent in 12- to 17-year-olds
- Traits: Like Pfizer’s vaccine, this one is mRNA-based, but it can be stored at -20 C. It’s approved for use in Canada for ages 12 and up.
- Also known as: Vaxzevria
- Approved on: Feb. 26, 2021
- Efficacy rate: 62 per cent two weeks after the second dose
- Traits: This comes in two versions approved for Canadian use, the kind made in Europe and the same drug made by a different process in India (where it is called Covishield). The National Advisory Committee on Immunization’s latest guidance is that its okay for people 30 and older to get it if they can’t or don’t want to wait for an mRNA vaccine, but to guard against the risk of a rare blood-clotting disorder, all provinces have stopped giving first doses of AstraZeneca.
- Also known as: Janssen
- Approved on: March 5, 2021
- Efficacy rate: 66 per cent two weeks after the single dose
- Traits: Unlike the other vaccines, this one comes in a single injection. NACI says it should be offered to Canadians 30 and older, but Health Canada paused distribution of the drug for now as it investigates inspection concerns at a Maryland facility where the active ingredient was made.
How many vaccine doses do I get?
All vaccines except Johnson & Johnson’s require two doses, though even for double-dose drugs, research suggests the first shots may give fairly strong protection. This has led health agencies to focus on getting first shots to as many people as possible, then delaying boosters by up to four months. To see how many doses your province or territory has administered so far, check our vaccine tracker for the latest numbers.
Canada has, to date, approved four vaccines. In clinical trials, the Pfizer vaccine had 95-per-cent efficacy against infection; Moderna 95 per cent; Johnson & Johnson 67 per cent; and AstraZeneca 62 per cent.
That doesn’t necessarily mean the Pfizer vaccine is way better than AstraZeneca. They measured efficacy slightly differently, and the trials happened at different times. Notably, the J&J and AstraZeneca vaccines were tested when variants had already begun to circulate.
Tracking Canada’s COVID-19 vaccine rollout plans: A continuing guide
All the vaccines seem to be a little less effective in protecting against variants, and that makes it all the more urgent that we vaccinate people as quickly as possible.
None of the vaccines is perfect. But all of them are close to 100-per-cent effective at preventing hospitalization and death. If there’s one statistic to remember as you head to the pharmacy for a shot, it’s that one.
If you read the news, you will know there are also a couple of other knocks against the AstraZeneca vaccine.
Some countries, like Canada, recommend that the AstraZeneca vaccine not be administered to people over 65. This recommendation, from the National Advisory Committee on Immunization, was “due to limited information,” meaning not many seniors were included in the clinical trials. In the real world, however, the AstraZeneca vaccine seems to be working well in all age groups.
As a result, many countries have overturned their earlier age-based restriction, and NACI will likely do the same in the coming days. Quebec is already using AstraZeneca vaccine for seniors.
It’s a reminder that experts can disagree, and that’s okay. Responding to a global pandemic is very much like building a plane in mid-flight: When you’re learning on the fly, some of the signals can be confusing.
Take the issue of blood clots as an example. In recent days, several countries have temporarily suspended the use of the beleaguered AstraZeneca vaccine due to reports of blood clots occurring after vaccination. Germany, France and Italy joined them on Monday.
This is likely a classic case of correlation not implying causation. More than 17 million people have received the AstraZeneca vaccine, and there have been 37 reports of blood clots, which is less than the background rate (the normal rate that blood clots happen, without the vaccine). So it’s likely a coincidence.
What we do know is that COVID-19 affects the circulatory system and blood clots occur far more often in the infected, which is another reason to get a vaccine.
The same correlation-versus-causation caution applies to stories about allergic reactions, seizures and deaths after vaccination. People have all manner of health problems; those don’t go away during a pandemic, nor are they necessarily exacerbated by vaccination.
Virtually everyone with allergies can safely get the vaccines. The only specific warnings are for those with a severe allergy to polyethylene glycol (PEG) to avoid the Pfizer and Moderna vaccines, and those allergic to polysorbate to avoid J&J’s product.
Another issue that has made headlines is the claim that coronavirus vaccines contain fetal tissue. That is incorrect. What is true is that cell lines derived from (voluntarily) aborted fetuses are used in the manufacturing of many vaccines and prescription drugs. The AstraZeneca vaccine uses the HEK-293 kidney cell line, which was derived from a fetus in 1972, and J&J uses the PER.C6 cell line (from 1985). While a few anti-choice zealots object, even the Vatican has said that Catholics can use medications derived from fetal cell lines in good conscience.
Still, Alberta Premier Jason Kenney says people should be able to refuse these vaccines for moral reasons. Other than being an oddly selective embrace of pro-choice views, it raises the question: Should Canadians be able to choose which coronavirus vaccine they get?
Theoretically, sure. But in practice, that would unduly complicate the rollout, for no good reason.
While there is a lot of noise out there, there is also a clear signal: Coronavirus vaccines are remarkably safe and effective. And the best vaccine is the one you can get into your arm.
Sign up for the Coronavirus Update newsletter to read the day’s essential coronavirus news, features and explainers written by Globe reporters and editors.