
Illustration by Romain Lasser
When Momar Ndao looks at the ingeniousness of the mRNA technology behind the COVID-19 vaccines, he sees hope in the fight against a category of diseases that blinded his mother and killed his uncle.
As a parasitologist and professor in the division of Experimental Medicine at McGill University, Dr. Ndao studies the worms and microscopic organisms that cause a slew of illnesses many Canadians may never have heard of. Schistosomiasis. Cryptosporidiosis. Chagas disease.
In wealthy countries, these blights are often referred to as neglected tropical diseases, but in poor ones like Dr. Ndao’s native Senegal, they are an ever-present fact of life.
Dr. Ndao was five when his mother lost her sight to onchocerciasis, a worm infection better known as river blindness. Decades later, an uncle who was like a second father to Dr. Ndao developed lymphatic filariasis, a roundworm infection that in his case caused elephantiasis of the testes. He was too ashamed to see a doctor and he died.
Watching the suffering of his family and friends in Senegal compelled Dr. Ndao to seek new treatments and vaccines for some of the 20 neglected diseases that, according to the World Health Organization, kill 200,000 people a year and sicken or maim tens of millions more.

Watching the suffering of his family and friends in Senegal compelled Dr. Ndao to seek new treatments and vaccines for neglected diseases.Fred Lum/The Globe and Mail
Although these illnesses don’t get the attention that COVID-19 does, they are devastating. Could the mRNA technology that reduced the death toll of the pandemic diminish their toll as well, Dr. Ndao wondered, as the success of these vaccines became apparent. He was far from the only scientist dreaming of how synthetic mRNA could transform their corner of medicine.
The COVID-19 vaccines developed by Moderna and Pfizer-BioNTech, both of which rely on mRNA created in a lab, have been hailed as a medical revolution. Their success has set off a tsunami of interest in using the technology to combat a Who’s Who of modern pestilences. Targets include influenza, Zika, HIV, malaria, cancer, heart disease, cystic fibrosis and “Disease X,” the placeholder name given to whatever yet-to-emerge illness fuels the next global health disaster.
Using mRNA (messenger ribonucleic acid) created in a laboratory, the groundbreaking COVID-19 vaccines teach cells to make a protein that triggers an immune response. They’re faster to produce than conventional vaccines, and the mRNA technology is infinitely reprogrammable. Diseases other than COVID-19 can, in theory, be tackled in similar ways – meaning that the potential applications of synthetic mRNA to prevent illness and treat diseases seems nearly limitless.
“The pandemic has been a total game-changer for the field,” Anna Blakney, a biomedical engineer at the University of British Columbia, said of mRNA science. Before COVID-19, most people had never heard of mRNA, she says. No company had completed a phase three trial of an mRNA product, let alone brought one to market. Now there are two approved mRNA vaccines that have been injected into the arms of hundreds of millions of people worldwide, providing the ultimate proof of concept for a technology that some doubted would ever be ready for prime time.
One of the most exciting projects in Dr. Ndao’s Montreal lab is an experimental vaccine for schistosomiasis, a disease that is second only to malaria in the pantheon of parasitic illnesses inflicting harm around the globe.

Mira Loock, an undergrad in Microbiology and Immunology at McGill University, works in the Cestari lab in April, 2022.Fred Lum/The Globe and Mail
But turning Dr. Ndao’s concept, which has shown promise in mice, into a safe and effective vaccine will be an immense scientific and logistical challenge – not to mention a financial one, considering how little profit there is to be turned from vaccines that only poor countries need.
Enter Moderna, Inc., the biotechnology company that shot to fortune and fame on the back of the COVID-19 vaccine it developed with the National Institutes of Health in the United States.
In early March, Moderna announced a global program called mRNA Access that will see the company share its vaccine-making recipe and ingredients with scientists working on emerging and neglected diseases. In return, those scientists will share research about the diseases they study, including potential targets for vaccines.
McGill was the first Canadian university to sign onto the framework in principle, and Dr. Ndao was among the first researchers to take part in preliminary meetings with company officials this spring. Not long after, Moderna announced a broader research partnership with the University of Toronto and confirmed it would build a vaccine factory in the Montreal area.
So far, Dr. Ndao and his colleagues have managed to provide strong, though not complete, protection against schistosomiasis in mice with a three-shot regimen made with older vaccine technology. He hopes that deploying mRNA technology against the target his lab has zeroed in on – a protein called Cathepsin B – will lead to a vaccine that offers “complete protection” against schistosomiasis.
In a study released in March, Dr. Blakney and her colleagues found 427 published papers that mentioned the term “RNA vaccine” in 2021, up from 99 in 2020 and next to none in the years before. The pipelines of the three best-known mRNA companies offer a glimpse of what lies ahead if clinical trials pan out. Excluding their COVID-19 products, Massachusetts-based Moderna, Germany’s BioNTech, and CureVac, another German company, have between them 41 human trials in progress, a handful of which are the kind of large, late-stage trials necessary for regulatory approval.

How the mRNA vaccines for
COVID-19 work
For more than 25 years, research labs have been exploring the use of messenger RNA to build the body’s immunity against diseases. With the technology’s proven efficacy against the COVID-19 virus, researchers see a future in which the platform could be used to make vaccines and treatments for many more diseases, including malaria, tuberculosis, hepatitis B, cystic fibrosis and even HIV, for which human trials of an mRNA vaccine have already begun.
The vaccine is a Messenger RNA (mRNA) encased in a lipid envelope
1
mRNA
Envelope
Cell membrane
HOST
CELL
The vaccine enters in a compartment (an endosome) formed from the cell membrane
2
The endosome fuses with the lipid envelope and the mRNA is released. The mRNA carries the instructions for making copies of the virus’ spike proteins
3
Ribosomes, the cell’s protein builders, read the mRNA and produce a long chain of amino acids called a polypeptide
4
Ribosome
Polypeptides
The polypeptides assemble to form the viral spike proteins
5
Viral spike protein
ACE2 receptors
The cell displays the spike proteins to the immune system
6
Antibody
The immune system is primed to produce antibodies that prevent the virus from attaching to host cells via the ACE2 receptor
7
Virus
particle
MURAT YÜKSELIR /
THE GLOBE AND MAIL

How the mRNA vaccines for COVID-19 work
For more than 25 years, research labs have been exploring the use of messenger RNA to build the body’s immunity against diseases. With the technology’s proven efficacy against the COVID-19 virus, researchers see a future in which the platform could be used to make vaccines and treatments for many more diseases, including malaria, tuberculosis, hepatitis B, cystic fibrosis and even HIV, for which human trials of an mRNA vaccine have already begun.
1
The vaccine is a Messenger RNA (mRNA) encased in a lipid envelope
mRNA
Envelope
Cell membrane
HOST CELL
2
The vaccine enters in a compartment (an endosome) formed from the cell membrane
3
The endosome fuses with the lipid envelope and the mRNA is released. The mRNA carries the instructions for making copies of the virus’ spike proteins
4
Ribosomes, the cell’s protein builders, read the mRNA and produce a long chain of amino acids called a polypeptide
Ribosome
Polypeptides
5
The polypeptides assemble to form the viral spike proteins
Viral spike protein
ACE2 receptors
6
The cell displays the spike proteins to the immune system
Antibody
7
The immune system is primed to produce antibodies that prevent the virus from attaching to host cells via the ACE2 receptor
Virus
particle
MURAT YÜKSELIR /
THE GLOBE AND MAIL

How the mRNA vaccines for COVID-19 work
For more than 25 years, research labs have been exploring the use of messenger RNA to build the body’s immunity against diseases. With the technology’s proven efficacy against the COVID-19 virus, researchers see a future in which the platform could be used to make vaccines and treatments for many more diseases, including malaria, tuberculosis, hepatitis B, cystic fibrosis and even HIV, for which human trials of an mRNA vaccine have already begun.
Virus
particle
The vaccine is a Messenger RNA (mRNA) encased in a lipid envelope
The immune system is primed to produce antibodies that prevent the virus from attaching to host cells via the ACE2 receptor
1
7
mRNA
Envelope
ACE2
receptors
Antibody
Cell membrane
The cell displays the spike proteins to the immune system
6
HOST CELL
Viral spike protein
The polypeptides assemble to form the viral spike proteins
5
The vaccine enters in a compartment (an endosome) formed from the cell membrane
2
Polypeptides
The endosome fuses with the lipid envelope and the mRNA is released. The mRNA carries the instructions for making copies of the virus’ spike proteins
Ribosomes, the cell’s protein builders, read the mRNA and produce a long chain of amino acids called a polypeptide
3
4
MURAT YÜKSELIR / THE GLOBE AND MAIL
The three companies have nearly three dozen more potential vaccines and medications in preclinical development. In BioNTech’s case, many are personalized cancer vaccines, the focus of the company’s research before it partnered with the pharmaceutical giant Pfizer to produce its COVID-19 vaccine. Moderna has candidates for influenza, RSV (a virus that can cause severe respiratory illness in the very young and very old) Zika, HIV and other viruses, along with bespoke cancer vaccines and prospective mRNA treatments for rare diseases.
Two of those medications are being tested at Toronto’s Hospital for Sick Children on a handful of kids with propionic acidemia and methylmalonic acidemia, a pair of rare inherited metabolic disorders with no good treatments. It’s early days for the trial, but Neal Sondheimer, the head of metabolic genetics at SickKids, is buoyed by how the mRNA treatments succeeded in animal testing.
“It’s heartening to me to be working on something that looks more into the future when these kids will do better and won’t get so sick,” he said.
Drew Weissman, the director of vaccine research at the University of Pennsylvania, said he’s lost count of all the mRNA projects his lab has on the go. The farthest along are five phase one trials: Two for HIV, two for influenza and one for genital herpes.
But the undertakings that excite him most are those that push the boundaries of mRNA science.
To cite one example, his lab is conducting animal experiments using mRNA technology to teach cells to fix damaged heart tissue. His team concocted an mRNA injection that prodded mice to produce Chimeric Antigen Receptor T cells, better known as CAR-T cells, that proved capable of repairing fibrosis on the hearts of mice. Treatments up until now have used CAR-T cells genetically engineered outside a patient’s body and injected as a form of personalized immunotherapy against certain blood cancers, a process that costs about half-a-million dollars per patient.
Hundreds of thousands of people die each year from neglected diseases, but the messenger RNA technology used in two COVID-19 vaccines opens the door for new treatments. Understand the principles of mRNA tech and meet the scientist from McGill University who hopes it will lead to an effective vaccine for a parasite-borne disease called schistosomiasis.
The Globe and Mail
The mouse experiments in Dr. Weissman’s lab, the results of which were published in the journal Science in January, suggest it might be possible, with a simple IV injection of mRNA, to teach the body to make its own CAR-T cells capable of repairing the scarring that is a hallmark of cardiac disease.
In other words, mRNA could reprogram T cells to fix a broken heart.
“We’re now taking that targeting and expanding it to many different types of treatments,” Dr. Weissman told The Globe and Mail, “for fibrosis of the liver and the lung, for treatment of lymphomas and leukemias, for treatment of autoimmunity, for many different things.”
Dr. Weissman’s lab is a hive of mRNA science for good reason: It was the birthplace of the modified mRNA used in both the Moderna and Pfizer-BioNTech COVID-19 vaccines.
When Dr. Weissman and his research partner, Katalin Kariko, a Hungarian-born biochemist who is now a senior vice-president at BioNTech, published details of their pivotal discovery in 2005, the wider scientific world didn’t pay much attention. Notoriously fragile and difficult to work with, mRNA seemed an impractical backbone for a new class of drugs.
Seventeen years and one devastating global pandemic later, the pair are considered likely candidates for a Nobel Prize.
A single-stranded molecule, mRNA delivers instructions from a cell’s DNA to its ribosomes, the cellular machines that make proteins. Dr. Kariko’s vision, which built upon earlier discoveries by other scientists, was to make synthetic mRNA that could tell cells to pump out any protein she chose, effectively converting the cells into microscopic medicine factories. (In the now familiar case of the COVID-19 vaccines, mRNA instructs the cells to produce a harmless piece of the spike protein found on the surface of the coronavirus, tricking the immune system into performing a dry run that readies it to fight the real virus.) If Dr. Kariko’s idea worked, future scientists would be able to plug the DNA sequence encoding for a specific protein into fancy lab equipment and watch as it spit out the right mRNA.
Taking that idea from theory to reality took decades of trial, error and rejection. Dr. Kariko first had to master the science of creating mRNA in a lab, then she and Dr. Weissman had to figure out why, against all expectations, their mRNA was making lab mice sick.
The rodents’ immune systems, it turned out, were greeting the synthetic mRNA as a foreign invader and mounting a dangerous inflammatory response. Dr. Kariko and Dr. Weissman’s solution was to rearrange the chemical bonds on one part of the mRNA, creating a modified molecule that tricked the immune system into lowering its defences. That was the breakthrough, published in their seminal 2005 paper, that made mRNA as medicine feasible.
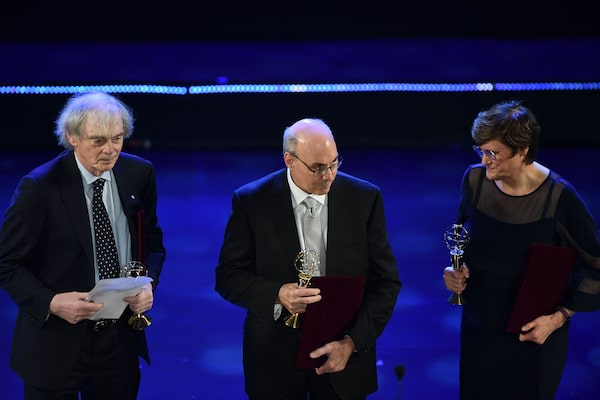
From left, scientists Pieter Cullis, Drew Weissman and Katalin Kariko stand on stage after receiving the 2022 Vinfuture Grand Prize for their work on mRNA technology.NHAC NGUYEN/AFP/Getty Images
The next crucial step was swaddling the modified mRNA in lipid nanoparticles, tiny globules of fat engineered primarily by University of British Columbia scientist Pieter Cullis. The lipid nanoparticles, now the subject of a messy patent fight among a handful of biotechnology companies with roots in UBC, delivered the fragile mRNA safely across the cell membrane.
Drs. Kariko, Weissman and Cullis were honoured last month with the Canada Gairdner International Award, a $100,000 accolade that has been a precursor to a Nobel prize for nearly 100 other scientists.
The speed of development and initial efficacy of the mRNA COVID-19 vaccines made the technology seem like an overnight success, but as Dr. Kariko told The Globe in an interview before receiving the Gairdner, in reality, “it took a zillion overnights.”

Noubar Afeyan, a chairman and co-founder of Moderna, at the Flagship Pioneering office in Cambridge, MA.Simon Simard/The Globe and Mail
The results, though, of those zillion overnights meant that when a new virus began circulating in China in late 2019, the handful of pharmaceutical companies with expertise in mRNA were primed to create a prototype vaccine faster than ever before.
It was a bitterly cold night in January of 2020, when Noubar Afeyan, Moderna’s chairman and one of its four co-founders, stepped away from his daughter’s birthday dinner to take a call from Stéphane Bancel, Moderna’s chief executive officer.
Mr. Bancel was in Switzerland at the Davos forum, where, as Dr. Afeyan recalled it, alarmed public health experts had “nearly accosted” him asking if there was anything Moderna could do about the mysterious pneumonia spreading in Wuhan.
The company had multiple mRNA vaccines in the works, including one against Middle East Respiratory Syndrome, a close cousin of the original SARS. Crucially, the platform was easily re-engineered; it was “always aimed at enabling a whole wide family of medicines,” said Dr. Afeyan, an entrepreneur whose family fled Lebanon’s civil war for Montreal when he was 13. As a teenager, he lived in a high-rise overlooking the McGill campus where he would later study chemical engineering.
Like their rivals at BioNTech, Moderna’s scientists made a prototype vaccine in a few days. Both shots proved safe and 95-per-cent efficacious at preventing symptomatic cases of COVID-19 in the pivotal phase-three trials that won them regulatory approval in less than a year, smashing all previous records for vaccine development. And once they began to be dispensed around the world at the end of 2020 and in early 2021, their ability to prevent severe illness and death proved to be a historic breakthrough.
When Omicron overcame the vaccines’ defences against mild infections, Pfizer-BioNTech and Moderna had to hasten their work on variant-specific boosters and a pan-coronavirus shot.ARND WIEGMANN/Reuters
Some of the shine has since come off those COVID-19 shots, less because of the vaccines themselves than the virus, which has cycled through progressively more contagious variants at speeds even the malleable mRNA vaccines can’t match.
Omicron punched the biggest hole yet in the vaccines’ defences against mild infections, spurring Pfizer-BioNTech and Moderna to hasten their work on variant-specific boosters and a pan-coronavirus shot. Fortunately, the existing COVID-19 shots are holding strong against severe illness and death, especially for those who’ve received three or more doses.
Still, the challenge raised by coronavirus variants is a reminder that, as high as hopes are for mRNA technology, there are good reasons for skepticism, too.
The biggest worry is that other pathogens may not be easy pickings for a vaccine the way SARS-CoV-2 was. Decades of research on the original SARS and MERS meant that by the time Chinese scientists sequenced SARS-CoV-2, it was well understood that a coronavirus’s spike protein would make a juicy target for a vaccine. The mRNA vaccines may have emerged as clear winners, but competing vaccines crossed the regulatory finish line as well, and they used more conventional approaches.
Jesse Clark, an infectious disease physician at UCLA’s school of medicine, said SARS-CoV-2 is simply not that complicated a foe. “In terms of complexity of the viral structure,” he said, “you’re looking at something that’s made at an elementary school level.”
By contrast, a pathogen such as HIV is an “advanced PhD level” opponent, ceaselessly mutating to defeat every previous attempt at a vaccine, Dr. Clark said. The latest failure was a Johnson & Johnson HIV candidate that used a defanged adenovirus as a delivery system for the vaccine’s payload – the same basic technology that worked in J & J’s COVID-19 vaccine.
As co-leader of an early-stage National Institutes of Health trial of three mRNA vaccines for HIV, Dr. Clark still sees promise in the platform. He just wants to temper expectations.
Patrick Ott, director of the Center for Personal Cancer Vaccines at the Dana Farber Cancer Institute in Boston, feels the same way. He’s wary of the hype surrounding bespoke mRNA cancer vaccines, most of which are plodding through small, early-stage trials.
Dr. Ott understands the concept is tantalizing: Sequence a patient’s tumour, insert the right code into the mRNA platform that curbed the pandemic, then inject a tailor-made vaccine that teaches the immune system to seek and destroy a unique cancer if it tries to recur.
Unfortunately, “cancer is just a totally different disease,” from COVID-19 and far harder to combat with a shot, he stressed. “It’s definitely a new world where we can do this now, “ with mRNA, he added, “but we have to figure out how to do it, and then it will take us some time to get there.”
Both Dr. Clark and Dr. Ott pointed out that, at the end of the day, mRNA is just an elegant messenger. Someone has to tell it what message to deliver, which proteins to order up. It requires a target.
That’s where the fundamental science undertaken by researchers such as McGill’s Dr. Ndao and his colleague, Igor Cestari, come in.

Dr. Ndao is researching parasitic worms that cause schistosomiasis, which thrive in rivers teeming with a certain type of freshwater snail.Fred Lum/The Globe and Mail
In his lab at the Research Institute of the McGill University Health Centre, Dr. Ndao holds up a glass jar of the parasites that cause schistosomiasis (they thrive in rivers teeming with a certain type of freshwater snail). The jar appears to hold nothing but water until Dr. Ndao shakes it, prompting dozens of wiggly, translucent flatworms the size of a fingernail cuticle to flicker into view. (Other specimens in his collection are easier to see. One is a coiled roundworm so large that lab workers have slapped the label “Big Bertha” on its jar.)
When the parasites pierce human skin, they maturate and the females produce eggs that travel to the intestine, liver or bladder, causing inflammation, fibrosis and scarring. Repeated infections, particularly in children who bathe and frolic in tropical rivers, lead to malnutrition, anemia and learning problems. Long-term untreated infections can also damage multiple organs, especially the liver.
There are no approved shots for parasitic diseases, save for one poor-performing vaccine for malaria.
Dr. Ndao, the long-time director of the National Reference Centre for Parasitology, and his fellow researchers found that suppressing a protein called Cathepsin B inhibited the ability of the parasites to digest red blood cells, starving them. Before the mRNA Access program came about, Dr. Ndao’s lab tested a three-dose vaccine using older technology that reduced the number of adult worms and eggs in mice by approximately 70 per cent, according to a study published in The Lancet’s eBioMedicine journal.
Dr. Ndao thinks an mRNA approach could work even better against Cathepsin B. It’s early days, but he’s looking forward to finding out if Moderna’s mRNA Access partnership lives up to its potential.
So is Dr. Cestari. His lab at McGill’s Institute of Parasitology is working on finding targets for a vaccine against Chagas disease, a parasitic infection first identified in his native Brazil. Left untreated, Chagas causes irreversible heart damage.
Dr. Cestari is leading a painstaking search for the best vaccine targets by slicing the DNA of the parasite that causes Chagas into millions of fragments and inserting those fragments into yeast. As the yeast grows, the parasite’s proteins are expressed on the surface of the yeast, allowing Dr. Cestari to bathe them in serum from the blood of Chagas patients to see what sticks. Seeing what sticks helps him to identify which proteins might make good targets for a vaccine.
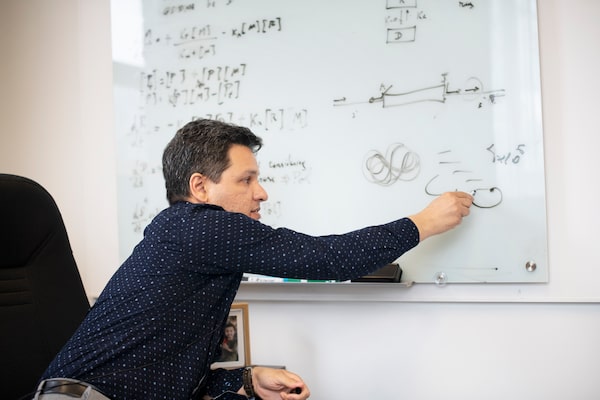
Igor Cestari, Assistant Professor at McGill’s Institute of Parasitology, is working on finding targets for a vaccine against Chagas disease, a parasitic infection first identified in his native Brazil.Fred Lum/The Globe and Mail
He has invested nearly two years of pandemic-interrupted labour to refine his list of the top 10 to 20 proteins to target. He’s nearly there now. The next step would be making his own prototype vaccine for Chagas, but if Moderna is willing to design one for him using their mRNA and his targets, development time could drop significantly.
“In theory, when I have the code, it’s as simple as sending a text message,” Dr. Cestari said, “and someone on the other side would put it in a machine to synthesize the RNA.”
Reality is more complicated. Dr. Cestari said he and McGill would want to patent the sequences of his targets before sharing them with Moderna. He would also want to hammer out terms on shared intellectual property with an eye to ensuring a future vaccine is affordable in the Central and South American countries where Chagas is endemic.
One of the discouraging lessons of the pandemic is that, in the event of an emergency, wealthy countries will snap up life-changing vaccines and treatments for their own populations first, neglecting the welfare of the developing world. Pharmaceutical companies, meanwhile, will always have profit margins and shareholders to think of first.
When it comes to ensuring tomorrow’s mRNA breakthroughs are available to those who need them most, publicly funded universities and scientists can do their part by writing equity access provisions into legal agreements with pharmaceutical companies, said Srinivas Murthy, a UBC critical care and infectious disease professor who co-chairs the WHO’s clinical research committee on COVID-19.
“The classic line is that we socialize all the risk, namely within the universities and researchers,” Dr. Murthy said. “Then, as soon as something is there, a company runs off and just develops it and recoups all the benefits.”
In interviews with The Globe, senior officials at Moderna Canada, McGill and the University of Toronto, all said the overarching research partnerships announced this spring were frameworks for co-operation. If any specific projects go forward they’ll be subject to individual legal agreements, the details of which are usually confidential.
For Dr. Cestari, the legal fine print is important, but not as important as the science itself. As the soft-spoken Brazilian moves around his Montreal lab, showing off petri dishes of yeast and scribbling on his white board to explain the mind-bending research he and his team are pursuing, his excitement at the thought of one day inventing a vaccine is infectious.
“You can see I’m a dreamer, right?” Dr. Cestari said. “I’m not shy of hope.”
With a report from Ivan Semeniuk
Sign up for the Coronavirus Update newsletter to read the day’s essential coronavirus news, features and explainers written by Globe reporters and editors.
 Kelly Grant
Kelly Grant