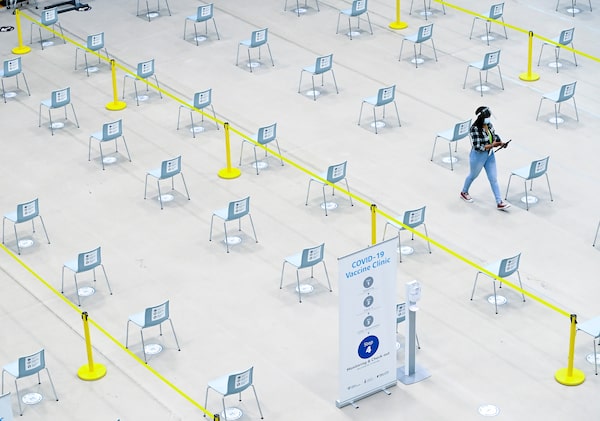
A worker walks through the empty waiting area at a mass COVID-19 vaccination clinic in Mississauga on March 1.Nathan Denette/The Canadian Press
Only three months ago, Prime Minister Justin Trudeau rose in the House of Commons and said that, when it came to vaccinations for COVID-19, Canada was in a superior position compared with its global peers.
The government’s planning, he said, “resulted in us having the best portfolio of vaccines of any country in the world, with more doses per capita than any other country.”
But as of this week, Canada ranked behind more than 30 countries in vaccination rates. Its number of inoculated citizens stalled in February, hovering at about 5 per cent – while peer countries such as Britain and the United States, as well as poorer countries such as Chile and Morocco, have accelerated their rollout.

Cumulative COVID-19 vaccination
doses administered
Per 100 people. This is counted as a single dose,
and may not equal the total number of people
vaccinated, depending on the specific
dose regime
100
Israel
80
60
40
Britain
U.S.
20
Chile
Morocco
Germany
Canada
0
15
Jan. 1
25
Feb. 4
14
March 1
the globe and mail, Source: Official data
collated by Our World in Data –
ast updated March 2

Cumulative COVID-19 vaccination
doses administered
Per 100 people. This is counted as a single dose, and
may not equal the total number of people vaccinated,
depending on the specific dose regime
100
Israel
80
60
40
Britain
U.S.
20
Chile
Morocco
Germany
Canada
0
15
Jan. 1
25
Feb. 4
14
March 1
the globe and mail, Source: Official data collated
by Our World in Data – Last updated March 2

Cumulative COVID-19 vaccination doses administered
Per 100 people. This is counted as a single dose, and may not equal the total number
of people vaccinated, depending on the specific dose regime
100
Israel
80
60
40
Britain
U.S.
20
Chile
Morocco
Germany
Canada
0
15
Jan. 1
25
Feb. 4
14
March 1
the globe and mail, Source: Official data collated by Our World in Data –
Last updated March 2
The government has assured Canadians the faltering start is now in the rearview mirror and a rapid increase in vaccine deliveries will see the country closing the gap.
On Wednesday, Mr. Trudeau said he was optimistic that Canada will be able to surpass his stated September deadline for getting shots to everyone. That end-of-summer deadline is in line with one set by Germany but behind Britain and the U.S.
How did the government go from proclaiming its performance was “the best” to fending off accusations that it had failed its citizens?
A Globe and Mail analysis has shown the Trudeau government’s lofty promises were never consistent with several hard realities: a severe lack of manufacturing capacity in a world obliged to vaccinate their own citizens first, as well as contracts with vaccine suppliers that appear to contain less-advantageous delivery schedules than those inked by Britain and the U.S.
What’s more, rather than prepare Canadians for an inevitable lag at the start of the vaccination schedule, the government relied on soaring rhetoric. It told Canadians it had hedged its bets and assured success by signing contracts with multiple international pharmaceutical giants. And although it’s certainly true that Ottawa placed wise bets on the vaccines first out of the clinical-trial gate – those developed by Pfizer-BioNTech, Moderna and Oxford-AstraZeneca – it didn’t properly explain to citizens that the global inoculation race had two distinct phases: first to purchase the vaccines and then to secure them.
“Canada, for some reason, was very quick to make purchases and really slow to invest in the manufacturing piece. I don’t know what went into those decisions,” said Andrea Taylor, a researcher with Duke University’s Global Health Innovation Centre, which has been tracking vaccine procurements around the world.
“They may have had more faith in the global supply chain than other countries.”

COVID-19 vaccinations: U.S. vs. Canada
As of March 2
Total vaccine doses administered per 100 persons
5
10
15
20
25
30
35
Gap in vaccination rates
The state with the lowest rate compared to the province with the highest rate
Alabama
19.6
7.9
PEI
MURAT YÜKSELIR / THE GLOBE AND MAIL, SOURCE: CDC; PROVINCIAL AND TERRITORIAL GOVERNMENTS

COVID-19 vaccinations: U.S. vs. Canada
As of March 2
Total vaccine doses administered per 100 persons
5
10
15
20
25
30
35
Gap in vaccination rates
The state with the lowest rate compared to the province with the highest rate
Alabama
19.6
7.9
PEI
MURAT YÜKSELIR / THE GLOBE AND MAIL, SOURCE: CDC; PROVINCIAL AND TERRITORIAL GOVERNMENTS

COVID-19 vaccinations: U.S. vs. Canada
As of March 2
Total vaccine doses administered per 100 persons
5
10
15
20
25
30
35
Alaska
Yukon
Nunavut
NWT
N.L.
B.C.
Alta.
Sask.
Man.
Que.
PEI
Ont.
N.B.
N.S.
Wash.
Maine
N.D.
Mont.
Minn.
N.Y.
Ore.
Vt.
Idaho
Wis.
Mich.
S.D.
N.H.
Pa.
Wyo.
Mass.
Iowa
Ohio
R.I.
Nebr.
Ind.
Ill.
W.Va.
Nev.
Conn.
Utah
Va.
Colo.
N.J.
Calif.
Ky.
Mo.
Kans.
Del.
N.C.
Tenn.
Md.
S.C.
Okla.
D.C.
Ark.
Ariz.
N.M.
Ga.
Ala.
Miss.
La.
Tex.
Fla.
Hawaii
Gap in vaccination rates
The state with the lowest rate compared to the province with the highest rate
Alabama
19.6
7.9
PEI
MURAT YÜKSELIR / THE GLOBE AND MAIL, SOURCE: CDC; PROVINCIAL AND TERRITORIAL GOVERNMENTS
Jockeying for position
The federal government was behind Britain and the U.S. in striking its first deals to buy the critical shots.
Coupled with the late appointment of a vaccine task force, Canada lost critical time, microbiologist Dr. Gary Kobinger said.
“By mid-February, [2020], it is clear we had an outbreak,” said Dr. Kobinger, who briefly sat on Ottawa’s vaccine task force. “Why were we not talking about a vaccine in February?”
Canada only decided to launch a vaccine task force after Britain and the U.S. had appointed theirs. Unlike other countries, Canada kept the existence of the task force, a volunteer group of about a dozen experts who recommended vaccine candidates, confidential for two months. It only formally announced the task force on Aug. 5.
The task force first met on June 16, but Dr. Kobinger said it wasn’t until July that they “really started talking about vaccines.” By then, he said, the vaccine candidates from AstraZeneca, Pfizer-BioNTech and Moderna were already well advanced.
In response to questions about the timing of the task force, John Power, a spokesperson for Industry Minister François-Philippe Champagne, wrote in an e-mailed statement, “a great deal of work was done to solicit credible scientific experts to volunteer their time to serve on it. Once established, they acted quickly, holding its first meeting on June 16th.”
Although Canada was one of the first countries to purchase promising vaccine candidates, those deals did not appear to guarantee priority access.
For instance, Canada was initially unable to negotiate guaranteed 2020 delivery from Pfizer – a promise Britain and the U.S. had secured from the pharmaceutical giant.
Later, however, Canada was able to extract 255,400 shots from Pfizer in December. In comparison, Britain received about five million shots from the company that month. The British task force credited these early shipments to being the first to strike a deal with Pfizer.
Although the federal government hasn’t released the contracts with the vaccine makers, there is an obvious inference to be drawn from the British experience, said Clint Hermes, a U.S.-based lawyer who advises the Coalition for Epidemic Preparedness Innovation, one of the organizations behind the international COVAX vaccine fund.
Britain, he said, was more successful at negotiating priority access – even though Britain, like Canada, does not manufacture the Pfizer-BioNTech vaccine itself.
“The U.K. just got a better deal,” Mr. Hermes said.

The Sanofi-Pasteur plant in Toronto's North York region is one of the two largest vaccine-production sites in Canada.Fred Lum/The Globe and Mail
Meagre manufacturing capacity
Back in the fall of 2020, Canada’s procurement strategy of hedging its bets was the subject of much scorn from international observers. The country had purchased enough vaccines to inoculate its citizens more than three times over, sparking accusations that it had undermined the ability of the developing world to order its fair share. In chart after chart displaying the leaders in global procurements, Canada was identified as the world’s worst hoarder.
But then, as vaccines started rolling off the assembly lines, Canada’s position on the new lists – those showing vaccinations in each country – plummeted.
“I remember thinking that was quite weird,” said Ms. Taylor, the Duke University researcher. One reason for Canada’s tailspin in the rankings is that other countries are using vaccines Canada isn’t considering, such as shots from China or Russia’s Sputnik V. However, Ms. Taylor said, Canada is missing a key ingredient: “Canada’s in a unique position, putting it at a disadvantage, which is there are very few high-income countries that don’t have at least a piece of the manufacturing.”
None of the vaccines approved by Health Canada thus far are manufactured in Canada. And for the time being, the country’s two largest vaccine production sites – a Toronto plant owned by Sanofi Pasteur, as well as a factory in Sainte-Foy, Que., owned by GlaxoSmithKline – will not be able to contribute much to Canada’s vaccination efforts.
Sanofi and GSK have partnered on a joint venture to develop their own COVID-19 vaccine, but poor results in their last clinical trial sent them back to the drawing board. (GSK is also working with Quebec’s Medicago on its vaccine candidate.) But even if the duo had succeeded, Sanofi has said it has no plans to use the Toronto plant for COVID-19 vaccines – the facility makes vaccines for diseases such as diphtheria and polio, which are supplied around the world. GSK supplies Canada with the flu shot and has kept pumping it out during the pandemic. If the vaccines GSK is working on are approved, it will make a component of the vaccines called the adjuvant (which helps stimulate the body’s immune response) at the Quebec plant.
Canada’s limited mass manufacturing took a key option off the table: making and stockpiling a vaccine before it was authorized.
In Britain, domestic AstraZeneca production has protected the country against the agonizing delays at Pfizer’s Belgian plant – delays that were acutely felt in Canada. Vaccines from the European plant are Canada’s only option, because the U.S. reserved the shots made within its borders. The AstraZeneca shot is the workhorse of the British vaccination plan, which has seen more than 30 per cent of the population receive their first dose.
Procurement Minister Anita Anand said all of the vaccine companies that Canada struck deals with in 2020 told the government they wouldn’t manufacture their shots here because the country lacked any mass-manufacturing options.
What Canada couldn’t do, others did. Lonza, the company contracted to manufacture ingredients for Moderna’s vaccine, used a novel approach to build – at a blistering pace – a production facility in Switzerland in 2020. The company constructed an empty factory and plugged in all the infrastructure – water, steam and gas – that is required for biomanufacturing.
Then, when Lonza signed a 10-year contract with Moderna in the spring, it was nearly ready to roll. “The empty shells allow us to drop in the manufacturing technology that is needed for a particular drug or vaccine,” Torsten Schmidt, who is leading the production facility in Switzerland, told the business magazine Fast Company. The Lonza plant was spitting out vaccines by November.
But in Canada, it wasn’t until August that Mr. Trudeau announced Ottawa was committing $126-million to a brand-new manufacturing facility in Montreal at the National Research Council (NRC). That funding was in addition to the $44-million the government previously committed to the NRC’s clinical-trial test facility in Montreal. The larger facility will mass-produce approximately two million vaccine doses a month. Neither facility will be able to supply shots as part of Canada’s 2021 vaccination plan, and the test facility is so delayed that the NRC has stopped giving a timeline for its completion.
Gérald André, an expert in biomanufacturing who is consulting with the NRC on the construction of the two facilities, said he is skeptical that Canada could have done more to increase capacity sooner.
“The short answer is no,” he said.
Canada Border Services Agency officers watch Canada's first shipment of the Moderna vaccine arrive by FedEx cargo jet on Dec. 24.Canada Border Services Agency/Handout via REUTERS
Kicking the can down the road
Canada needed to strike deals with foreign multinationals, in part because it ignored for decades numerous warnings about the need for a bolstered national immunization strategy. The latter was a key recommendation of a group that was convened to tackle the HIV epidemic in 1993. A decade later, calls for such a strategy were repeated in the definitive report on the SARS outbreak, which was authored by a group led by David Naylor, a former president of the University of Toronto.
“With each passing month, it gets more frustrating to reread that report,” Dr. Naylor, who is advising the federal government as co-chair of its COVID-19 Immunity Task Force, told The Globe.
That 2003 report was prescient, pointing out Canada’s patchwork of strategies “limit the security of vaccine supply.”
Dr. Naylor and his team called on Ottawa to earmark at least $100-million a year for a national strategy and suggested the federal government should partner with the private sector for “vaccine research and development, as well as production in Canada.”
On Feb. 25, The Globe asked the Public Health Agency of Canada for the budget of the national immunization strategy and its vaccination program. A week later, it has yet to provide the information.
Various proposals have been made about how to build domestic capacity. Joel Lexchin, a health-policy expert who testified this month at a House of Commons committee, called on Ottawa to keep vaccine-making public.
“We need to invest in a domestic, publicly owned vaccine-manufacturing facility so that we can avoid the situation of a privately owned Canadian company being sold to foreign interests at some time in the future, and therefore removing control from Canadian hands,” he told parliamentarians.

People wait in line for vaccines at Montreal's Olympic Stadium on March 1.Paul Chiasson/The Canadian Press
David vs. Goliath
While major drug makers turned down the federal government’s search for a domestic manufacturing solution, much smaller groups in Canada were clamouring for federal funding – and say they could have been further ahead and making shots domestically this year.
Dr. Kobinger, who heads the Infectious Disease Research Centre at Laval University in Quebec, said his team had a vaccine candidate that would be much closer to approval had they received more funding. Instead, he received almost $1-million from the federal government in March, and the vaccine is in early development.
Canada did invest in domestic vaccine development and manufacturing projects last year, but Dr. Kobinger said the sums were modest and much more could have been done to speed up the process and prioritize potential homegrown candidates. He said Canada missed the chance for a partnership similar to the University of Oxford-AstraZeneca vaccine, where the university’s team developed the vaccine and the pharmaceutical giant was responsible for mass manufacturing.
His comments were echoed by Amine Kamen, a McGill University professor and Canada Research Chair in Bioprocessing of Viral Vaccines. Dr. Kamen said the expertise in Canada is “highly comparable” to that in Britain, but part of the problem was the federal government lacked the political will and was risk-averse.
Calgary-based vaccine developer Providence Therapeutics said it has been warning the government since last spring about the risk of vaccine nationalism and highlighting the need for a domestic option. Like Pfizer and Moderna, Providence is also making an mRNA vaccine. In an interview with The Globe, chief executive officer Brad Sorenson said the company asked Ottawa for $35-million to help speed up its clinical trials last spring and line up domestic manufacturing at the same time.
Since then, his company has inked a deal with a Manitoba manufacturer, Emergent BioSolutions, to produce the shots, Mr. Sorenson said. In a statement, Emergent said its facility has been approved by Health Canada and is able to produce Providence’s mRNA vaccine. The federal government does not have a deal to buy shots from Providence. In February, the Manitoba government said it would buy two million doses of the company’s vaccine.
Similarly, John Lewis, CEO of Edmonton’s Entos Pharmaceuticals, told a parliamentary committee in February that it was a “mistake” not to invest more in these homegrown candidates still under development.
But Ottawa’s 11-member vaccine task force, which was comprised of scientists and former pharmaceutical executives, says there were simply no small vaccine developers in Canada that could be ready by September – which is when the Prime Minister has said every Canadian should be able to get vaccinated by. (Only one of the seven procurement deals that Ottawa signed – deals recommended by the task force – was with a Canadian developer, Medicago. The Quebec City company’s vaccine candidate is in the final stage of clinical trials.)
Mark Lievonen, the task force co-chair, said in an interview that his team’s mandate was to select effective vaccines that could be delivered to Canadians as soon as possible. In keeping with that directive, one of the criteria his group used to make recommendations was whether any of the potential vaccines had made it to the first phase of clinical trial. Mr. Lievonen declined to discuss individual companies, but said no small Canadian companies were that far along.
“I think it would be challenging for a small Canadian company to advance that quickly through the stages to get a vaccine faster than the ones that have been procured,” Mr. Lievonen said. He also pointed out that many smaller companies received some support from a $23-million fund that was made available through Ottawa’s Industrial Research Assistance Program. That level of funding, he said, “is probably consistent with the stage of development that they were at.”
Mexico's deputy foreign minister welcomes a container of ingredients for China's CanSino vaccine in Mexico City on Feb. 11. A planned joint project to test the vaccine in Canada fell apart last year.Mexico's Foreign Minister/Handout via REUTERS
An early bet doesn’t pay off
One of Canada’s first moves to secure vaccines fell flat – because of a combination of geopolitics and science.
On May 12 of last year, the National Research Council of Canada announced it had struck a deal with CanSino Biologics, a Chinese pharmaceutical company that had ties to the NRC.
The deal was supposed to result in CanSino supplying researchers at Dalhousie University with samples of its vaccine to conduct human trials in Canada, with a view to manufacturing the vaccines at NRC facilities. The deal was seen as a coup, as CanSino’s vaccine candidate was the first in the world to move into the second stage of clinical trials. An NRC executive, Roman Szumski, said the deal would position Canada to be “part of the front-runner story.”
But within a week, the deal was dead.
The federal government learned on May 19 that a shipment of CanSino’s candidate vaccine seeds were detained by customs at the Beijing Capital International Airport. The seeds, a necessary ingredient to developing a vaccine, never made it to Canada. What role Canada’s current icy relations with China played in this move, if any, has never been disclosed. In 2018, Chinese authorities detained two Canadian citizens, which Mr. Trudeau has called retaliation for the RCMP’s arrest of Huawei executive Meng Wanzhou at the request of the U.S.
Had the seeds even made it to Halifax, the joint venture would not have done much to improve Canada’s vaccination standing.
The vaccine task force, which was launched after the NRC signed its deal with CanSino, had initial concerns about the effectiveness of the vaccine’s model, task force member Alan Bernstein told parliamentarians. When data from the clinical trials rolled in during the summer of 2020, they confirmed the group’s fears, he said. “We then recommended that the collaboration end.”
Dr. Kobinger was much more blunt in his assessment. He said the vaccine was an outdated model, adding that whoever decided to get behind it was “somebody who … clearly does not know much about vaccines.”
As for who wears the blame for the CanSino decision, the NRC said in a statement the deal “was signed by the NRC on its own authority,” but acknowledged it “consulted” with the Ministry of Innovation, Science and Economic Development before finalizing the agreement.
With a report from Paul Waldie
/cloudfront-us-east-1.images.arcpublishing.com/tgam/HHZJFWHEBVP2PNLXDUQCLLLQIE.jpg) COVID-19 vaccine tracker: Canada’s rollouts compared
COVID-19 vaccine tracker: Canada’s rollouts compared
How big is the vaccine supply? How many doses have been administered? How does Canada’s vaccination rate stack up against the U.S.’s or Britain’s? Check our data page for the latest numbers.